Background
Allogeneic hematopoietic cell transplantation (allo-HCT) remains the only potentially curative treatment option for patients with myelodysplastic syndrome (MDS). The use of PTCY for GVHD prevention is becoming increasingly prevalent across donor types/transplant platforms. However, limited studies have evaluated the efficacy and safety of using PTCY in patients with MDS undergoing matched sibling donor (MSD) allo-HCT. We hereby compare the outcomes of PTCY-based versus (vs.) conventional GVHD prophylaxis in a contemporaneous cohort of MDS patients undergoing MSD allo-HCT from the EBMT registry.
Methods
A total of 404 MDS patients undergoing first MSD peripheral blood allo-HCT between 2014 and 2020 in 52 participating centers, receiving either PTCY or other GvHD prophylaxis, were included. Primary outcomes were overall survival (OS), progression free survival (PFS), GVHD-free/RFS (GRFS), competing risks analyses for relapse (CIR), non-relapse mortality (NRM), and GVHD. The main comparison was PTCY vs. other types of GvHD prevention. Cox regression analyses with predefined covariates were used to obtain adjusted effect estimates of PTCY in post-transplant results.-
Results
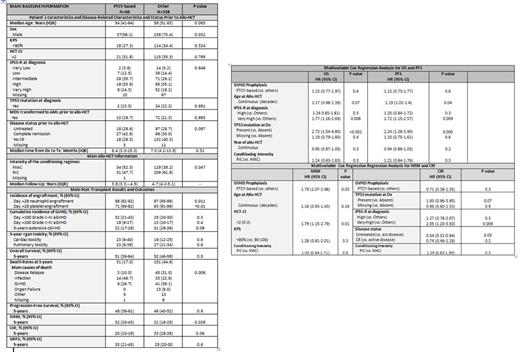
The median age at allo-HCT was 57 years (IQR 49-62), 66 patients (16.3%) received PTCY, 338 (83.7%) received other prophylaxis. As reported in Figure 1, patient characteristics, disease risk, and pre-transplant status were balanced between the two cohorts. The majority of transplant characteristics were also analogous except for the proportion of adults receiving myeloablative regimens, which was higher in the PTCY group (52.3% vs. 38.2%, P=0.047).
PTCY was combined with two additional immunosuppressant agents in 66.7% of the cases, with one additional immunosuppressive drug (generally calcineurin inhibitors (CNI)) in 31.8%, and administered as a single agent in only 1 (1.5%) case. Other prophylaxis mainly combined CNI with either mycophenolate mofetil or methotrexate, and in 162 (47.9%) of the cases, anti-thymocyte globulin was also administered.
Post-transplant complications and outcomes are shown in Figure 1. Incidences of Day +28 neutrophil (68% vs. 97%, P=0.011) and platelet (71% vs. 92%, P<0.001) engraftment were lower in patients who received PTCY. The day +100 cumulative incidences (CI) of grade II-IV and III-IV aGVHD, and 5-year CI of extensive cGVHD were 32% (21-43%), 18% (9-27%) and 18% (9-28%) for patients who received PTCY, and 25% (20-30%; p=0.3), 13% (10-17%; p=0.4), 31% (26-36%; p=0.09) for those who did not. The 5-year CIs of cardiac and pulmonary toxicities were similar in both groups (23% (6-40%) vs. 19% (12-25%) (p=0.6) and 23% (8-38%) vs. 27% (21-34%) (p=0.6) in PTCY vs others, respectively). At 5-years after allo-HCT, the estimated OS (51% (39-64%) vs. 52% (46-58%), p=0.6), PFS (48% (36-61%) vs. 46% (40-52%), p=0.9), and GRFS (33% (21-45%) vs. 25% (20-30%), p=0.6), were similar between the two study groups. Nevertheless, patients who received PTCY tended to have lower CIR (20% (10-29%) vs. 33% (28-38%) (p=0.06)), but higher NRM rates (32% (20-43%) vs. 21% (16-25%), p=0.09) than the rest.
Next, we performed a multivariable analysis (MVA) of OS, PFS, NRM and CIR (Figure 1). The results observed in the MVA confirmed that using PTCY in patients with MDS undergoing MSD allo-HCT resulted in comparable OS (HR 1.23 (0.77-1.97), p=0.4) and RFS (HR 1.13 (0.73-1.77), p=0.6) to conventional prophylaxis. Furthermore, the diagnosis of a high or very high-risk MDS (according to IPSS-R), and the presence of TP53 mutation at diagnosis were independent predictors of worse post-transplant outcomes. In addition, PTCY-based prophylaxis was associated with a higher NRM (HR 1.79 (1.07-2.98), p=0.03) when adjusted by variables known to be clinically relevant for NRM.
Conclusion
The use of PTCY in adults undergoing MSD allo-HCT for MDS resulted in comparable OS and RFS rates to conventional GVHD prophylaxis. Allo-HCT performed with PTCY was associated with a longer time to engraftment and comparable incidences of clinically relevant aGVHD. Of note, utilization of PTCY was associated with a non-significant trend to a lower incidence of extensive cGVHD. Furthermore, although a non-significant trend to lower rates of relapse were observed in allo-HCTs performed using PTCY, it use was associated with a higher risk for NRM. Further evaluation of PTCY in the MSD setting for MDS is required.
Disclosures
Finke:Gilead Sciences: Current holder of stock options in a privately-held company; Riemser: Honoraria, Research Funding, Speakers Bureau; Neovii: Honoraria, Research Funding, Speakers Bureau; AbbVie: Current holder of stock options in a privately-held company; Roche: Current holder of stock options in a privately-held company; Medac: Honoraria, Research Funding. Platzbecker:MDS Foundation: Membership on an entity's Board of Directors or advisory committees; Curis: Consultancy, Research Funding; Geron: Consultancy, Research Funding; Roche: Research Funding; Servier: Consultancy, Honoraria, Research Funding; Silence Therapeutics: Consultancy, Honoraria, Research Funding; Syros: Consultancy, Honoraria, Research Funding; Celgene: Honoraria; BeiGene: Research Funding; AbbVie: Consultancy; Jazz: Consultancy, Honoraria, Research Funding; Merck: Research Funding; Fibrogen: Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Research Funding; Bristol Myers Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel support; medical writing support, Research Funding; Janssen Biotech: Consultancy, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; BMS: Research Funding. McLornan:UK ALL RIC TRIAL - DSM board: Other: participation on a data safety monitoring board or advisory board; Novartis: Honoraria; EBMT Scientific Council Member: Other: Chair of EBMT CMWP; Jazz Pharma: Honoraria; Abbvie: Honoraria; Imago Biosciences: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal